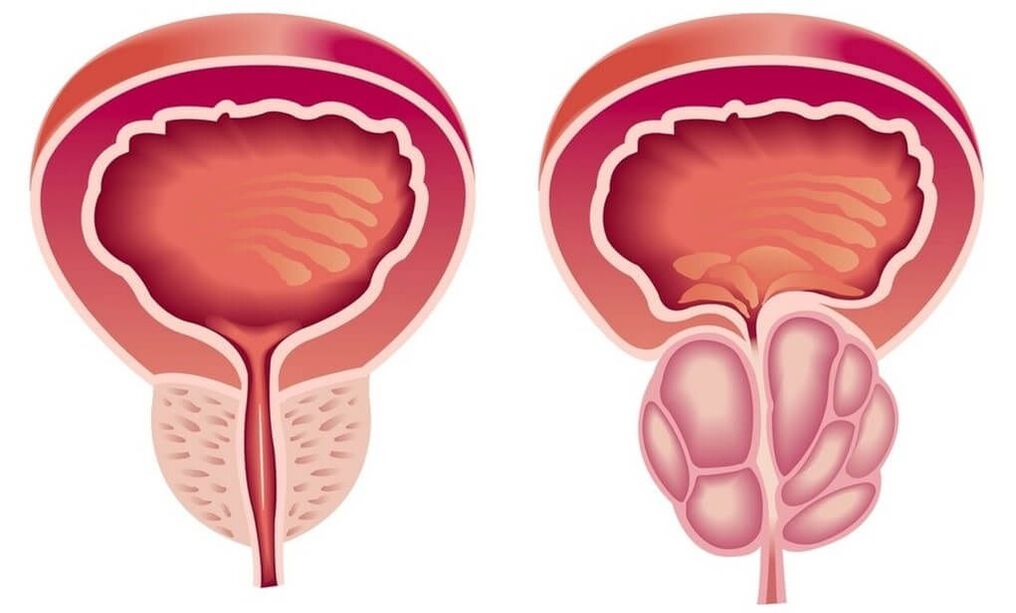
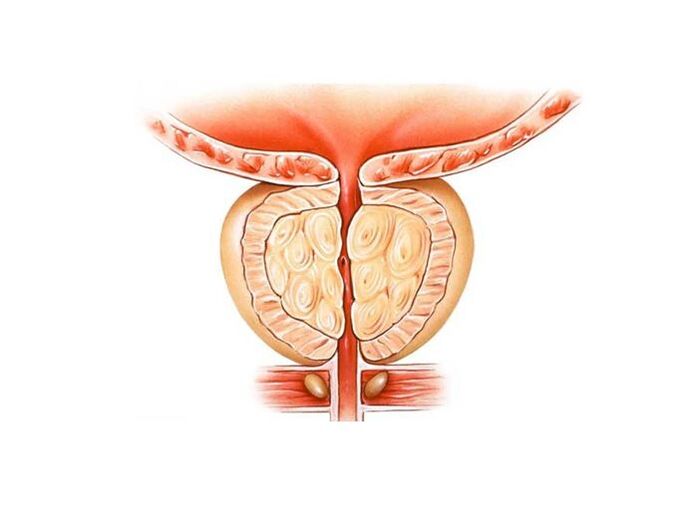
Prostatitisis an inflammatory disease of the prostate. Manifested by frequent urination, pain in the penis, scrotum, rectum, sexual disorders (erection dysfunction, premature ejaculation, etc. ), sometimes urinary retention, blood in the urine. The diagnosis of prostatitis is established by a urologist or an andrologist according to a typical clinical picture, the results of a digital rectal examination. Additionally, ultrasound of the prostate, bakposev of prostatic secretion and urine is performed. Treatment is conservative - antibiotic therapy, immunotherapy, prostate massage, lifestyle correction.

general informations
Prostatitis is an inflammation of the seminal gland (prostate) - the prostate. It is the most common disease of the genitourinary system in men. Most often affects patients aged 25-50 years. According to various data, 30-85% of men over 30 suffer from prostatitis. Possible formation of prostate abscess, inflammation of the testicles and appendages, which threatens infertility. The rise of the infection leads to inflammation of the upper genitourinary system (cystitis, pyelonephritis).
Pathology develops with the penetration of an infectious agent that enters the prostate tissue from the organs of the genitourinary system (urethra, bladder) or from a distant inflammatory focus (with pneumonia, influenza, tonsillitis, furunculosis)
Causes of prostatitis
As an infectious agent in an acute process, Staphylococcus aureus (Staphylococcus aureus), Enterococcus (Enterococcus), Enterobacter (Enterobacter), Pseudomonas (Pseudomonas), Proteus (Proteus), Klebsiella (Klebsiella) and Escherichia coli (E. Coli)can act. Most microorganisms belong to the conditionally pathogenic flora and cause prostatitis only in the presence of other predisposing factors. Chronic inflammation is usually due to polymicrobial associations.
The risk of developing the disease increases with hypothermia, a history of specific infections, and conditions accompanied by congestion in the tissues of the prostate. There are the following predisposing factors:
- General hypothermia (temporary or permanent, related to working conditions).
- A sedentary lifestyle, a specialty that requires a person to sit for a long time (computer scientist, driver, etc. ).
- Constant constipation.
- Violations of the normal rhythm of sexual activity (excessive sexual activity, prolonged abstinence, incomplete ejaculation during "usual" sexual intercourse devoid of emotional coloring).
- The presence of chronic diseases (cholecystitis, bronchitis) or chronic infectious foci in the body (chronic osteomyelitis, untreated caries, tonsillitis, etc. ).
- Past urological diseases (urethritis, cystitis, etc. ) and sexually transmitted diseases (chlamydia, trichomoniasis, gonorrhea).
- Conditions that cause immune system suppression (chronic, irregular stress and malnutrition, lack of regular sleep, overtraining in athletes).
It is assumed that the risk of developing pathology increases with chronic intoxication (alcohol, nicotine, morphine). Some studies in the field of modern andrology prove that chronic perineal trauma (vibration, concussion) in motorists, bikers and cyclists is a provoking factor. However, the vast majority of experts believe that all these circumstances are not the real causes of the disease, but only contribute to the exacerbation of the latent inflammatory process in the tissues of the prostate.
A decisive role in the onset of prostatitis is played by congestion of prostate tissue. Violation of capillary blood flow causes increased lipid peroxidation, edema, exudation of prostate tissues and creates conditions for the development of an infectious process.
Symptoms of prostatitis
Acute prostatitis
There are three stages of acute prostatitis, which are characterized by the presence of a certain clinical picture and morphological changes:
- Acute catarrhal. Patients complain of frequent and often painful urination, pain in the sacrum and perineum.
- Acute follicular. The pain becomes more intense, sometimes radiating to the anus, aggravated by defecation. Urination is difficult, urine flows in a thin stream. In some cases, there is urinary retention. A subfebrile state or moderate hyperthermia is typical.
- Acute parenchymal. Severe general intoxication, hyperthermia up to 38-40°C, chills. Dysuric disorders, often - acute urinary retention. Sharp and shooting pains in the perineum. Difficulty defecating.
Chronic prostatitis
In rare cases, chronic prostatitis becomes the result of an acute process, however, as a rule, a primary chronic course is observed. The temperature sometimes rises to subfebrile values. The patient notes a slight pain in the perineum, discomfort during the act of urination and defecation. The most characteristic symptom is scanty discharge from the urethra during defecation. The primary chronic form of the disease develops over a considerable period of time. It is preceded by prostatosis (blood stagnation in the capillaries), gradually transforming into abacterial prostatitis.
Chronic prostatitis is often a complication of the inflammatory process caused by the causative agent of a specific infection (chlamydia, trichomonas, ureaplasma, gonococcus). Symptoms of a specific inflammatory process in many cases mask the manifestations of prostate damage. Perhaps a slight increase in pain during urination, slight pain in the perineum, little discharge from the urethra during defecation. A slight change in the clinical picture often goes unnoticed by the patient.
Chronic inflammation of the prostate can be manifested by a burning sensation in the urethra and perineum, dysuria, sexual disorders, increased general fatigue. The consequence of violations of potency (or fear of these violations) often becomes mental depression, anxiety and irritability. The clinical picture does not always include all listed symptom groups, differs between patients and changes over time. There are three main characteristic syndromes of chronic prostatitis: pain, dysuria, sexual disorders.
There are no pain receptors in prostate tissue. The cause of pain in chronic prostatitis becomes almost inevitable due to the abundant innervation of the pelvic organs, involvement in the inflammatory process of the nerve pathways. Patients complain of pain of varying intensity - from weak and painful sleep to intense and disturbing sleep. There is a change in the nature of the pain (intensification or weakening) with ejaculation, excessive sexual activity or sexual abstinence. The pain radiates to the scrotum, sacrum, perineum, sometimes to the lumbar region.
As a result of inflammation in chronic prostatitis, the volume of the prostate increases, compressing the urethra. The lumen of the ureter is reduced. The patient has frequent urges to urinate, a feeling of incomplete emptying of the bladder. As a rule, dysuric phenomena are expressed in the early stages. Then, a compensatory hypertrophy of the muscle layer of the bladder and ureters develops. Symptoms of dysuria during this period weaken, then increase again with the decompensation of adaptive mechanisms.
In the early stages, dyspotence may develop, which manifests differently in different patients. Patients may complain of frequent nocturnal erections, blurry orgasm, or worsening erections. Accelerated ejaculation is associated with a decrease in the orgasmic center arousal threshold. Painful sensations during ejaculation can cause refusal of sexual activity. In the future, sexual dysfunctions become more pronounced. In the advanced stage, impotence develops.
The degree of sexual disorder is determined by many factors, including the patient's sexual constitution and psychological mood. Violations of potency and dysuria can be due both to changes in the prostate gland and to the suggestibility of the patient, who, if he has chronic prostatitis, expects the inevitable development of sexual disorders and disorders ofurination. Especially often, psychogenic dyspotence and dysuria develop in suggestible and anxious patients.
Impotence, and sometimes even the threat of possible sexual disorders, is difficult for patients to tolerate. Often there is a change of character, irritability, obnoxiousness, excessive concern for one's own health, and even "care of illness. "
Complications
In the absence of timely treatment of acute prostatitis, there is a significant risk of developing a prostate abscess. With the formation of a purulent focus, the patient's body temperature rises to 39-40 ° C and can become hectic in nature. Periods of heat alternate with violent chills. Sharp pains in the perineum make urination difficult and defecation impossible.
Increased prostatic edema leads to acute retention of urine. Rarely, an abscess ruptures spontaneously in the urethra or rectum. When opened, purulent, cloudy urine with an unpleasant pungent odor appears in the urethra; when opened, the feces contain pus and mucus in the rectum.
Chronic prostatitis is characterized by an undulating course with periods of long-term remissions, during which the inflammation of the prostate is latent or manifests itself with extremely weak symptoms. Patients who are not bothered by anything often stop treatment and only turn around when complications develop.
The spread of infection through the urinary tract provokes the appearance of pyelonephritis and cystitis. The most common complication of the chronic process is inflammation of the testicles and epididymis (epdidymo-orchitis) and inflammation of the seminal vesicles (vesiculitis). The result of these diseases is often infertility.
Diagnostic
The characteristic clinical picture simplifies the diagnostic process in acute and chronic prostatitis. It is mandatory to:
Treatment of prostatitis
Treatment of acute prostatitis
Patients with an uncomplicated acute process are treated by an outpatient urologist. In case of severe poisoning, suspicion of a purulent process, hospitalization is indicated. Antibacterial treatment is carried out. Preparations are selected taking into account the susceptibility of the infectious agent. Antibiotics are widely used and can penetrate prostate tissue well.
With the development of acute urinary retention against the background of prostatitis, they resort to the installation of a cystostomy, and not a urethral catheter, since there is a risk of the formation of a prostate abscess. With the development of an abscess, a transrectal or transurethral endoscopic opening of the abscess is performed.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should be complex, including etiotropic therapy, physiotherapy, correction of immunity:
- Antibiotic therapy. The patient is prescribed long courses of antibacterial drugs (within 4-8 weeks). The selection of the type and dosage of antibacterial drugs, as well as the determination of the duration of treatment are carried out individually. The drug is selected based on the sensitivity of the microflora based on the results of urine culture and prostate secretion.
- Prostate massage.Massage of the gland has a complex effect on the affected organ. During the massage, the inflammatory secret accumulated in the prostate is expelled through the ducts, then enters the urethra and is evacuated from the body. The procedure improves blood circulation in the prostate, which minimizes congestion and ensures better penetration of antibacterial drugs into the tissues of the affected organ.
- Physiotherapy.To improve blood circulation, laser exposure, ultrasonic waves and electromagnetic vibrations are used. If it is impossible to perform physiotherapeutic procedures, the patient is prescribed warm medicinal microclysters.
In long-term chronic inflammation, consultation with an immunologist is indicated to select immunocorrective treatment tactics. The patient receives advice on lifestyle changes. Making certain changes in the lifestyle of a patient with chronic prostatitis is both curative and preventive. The patient is recommended to normalize sleep and wakefulness, establish a diet, conduct moderate physical activity.
For the treatment of prostatitis, antibiotic therapy is the most effective. Phytotherapy, immunocorrectors and hormonal preparations can also be used on medical prescription.
In the absence of acute symptoms, prostatitis can be treated with physiotherapy methods. In case of abscesses and suppuration, surgery is recommended.
Treatment with drugs
Treatment of prostatitis with antibiotic therapy should begin with bakposev, the purpose of which is to assess the body's sensitivity to this type of antibiotic. In violation of urination, a good result is the use of anti-inflammatory drugs.
Drugs are taken in the form of tablets, in acute cases - in the form of droppers or intramuscularly. For the treatment of chronic forms of prostatitis, rectal suppositories are effective: with their help, drugs achieve their goal faster and have a minimal effect on other organs.
Anticoagulants and anti-inflammatories have also been proven.
Antibacterial therapy
Antibiotics are an effective remedy in the fight against bacterial prostatitis. In order to achieve the desired effect and not harm the body, the choice of drug, dosage and treatment regimen should be made by a doctor. To correctly select the most effective drugs, he will have to find out what kind of pathogen caused prostatitis, and also check the patient's tolerance to antibiotics of a particular group.
For the effective treatment of chronic prostatitis, antibiotics from the group of fluoroquinolones have proven themselves. Their action is aimed at suppressing a bacterial infection and strengthening the body's own immunity. In addition, a bacteriostatic antibiotic is recommended for the prevention and treatment of concomitant diseases of the genitourinary system.
Treatment of prostatitis caused by mycoplasmas and chlamydia can also be done with macrolides and tetracyclines, which slow the spread of infection.
The duration of taking antibacterial drugs is 2-4 weeks. In case of positive dynamics, the course can be extended.
Physiotherapy
Physiotherapeutic methods in the treatment of prostatitis are aimed at activating blood circulation in the pelvic region, improving metabolic processes in the prostate and cleaning the ducts. If physiotherapy is combined with taking antibiotics, the effect of the latter is enhanced.
The main methods include:
- magnetic therapy;
- laser therapy;
- electrophoresis;
- warming up;
- ultrasound;
- mud treatment;
- high frequency irradiation;
- physiotherapy.
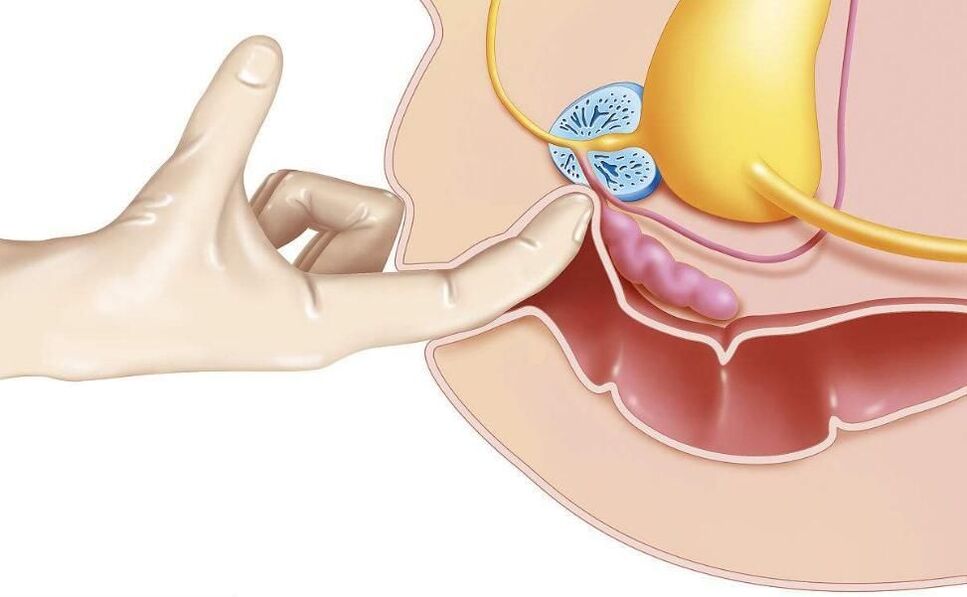
One of the oldest methods - transrectal prostate massage, according to modern research, has no proven effectiveness.
Non-specific treatments
Non-specific treatments for prostatitis include:
- hirudotherapy;
- curative fasting;
- acupuncture;
- diet according to the Ostrovsky method;
- alkalization of the body according to the method of Neumyvakin.
It is strongly recommended that you coordinate all non-traditional methods of treating prostatitis with your doctor.
Surgery
Surgical methods are used in complex and emergency cases:
- for the drainage of purulent abscesses, which are removed by laparoscopic methods through a puncture;
- in violation of urination due to damage to the urinary tract;
- with a large volume of the affected area;
- with a significant number of stones in the body of the gland.
Stones and sclerotic tissue are removed by endoscopic methods. With a large damaged area or several stones, resection of the prostate is resorted to.
Transurethral resection is also effective for bacterial prostatitis. Thus, it is possible to reduce the risk of relapse.
Folk remedies
The treatment of prostatitis with folk remedies is unlikely to be effective on its own, but in combination with medical and physiotherapeutic methods it may be applicable. These include: bee products, decoctions of herbs and seeds, tinctures of garlic, ginger, beaver brook, fresh vegetables, pumpkin seeds.
In acute cases of the course of the disease, you need to consult a doctor, and in no case should you self-medicate! In case of rupture of a purulent abscess, a fatal outcome is possible.
Candles for prostatitis
Treatment of prostatitis with rectal suppositories is much more effective than tablets, if only because the rectum is much closer to the prostate, which means that the drug will act faster.
The composition of drugs for the treatment of prostatitis can be completely different, they are prescribed to solve a particular problem.
- Antibacterial agents are especially effective for prostatitis caused by chlamydia.
- Analgesics are used for symptomatic treatment, they relieve pain well.
- Immunostimulants improve blood circulation, relieve swelling and are used in complex therapies.
- Phytopreparations have a mild effect. They, like candles on bee products, are used as an addition to the main treatment.
- Compositions based on ichthyol promote blood circulation in the area of the intestinal mucosa, which accelerates the attenuation of inflammatory processes and slightly improves immunity.
- Enzyme products prevent the formation of scar tissue. It is recommended to take as part of a complex therapy with antibiotics, anti-inflammatory and painkillers.
Auxiliary drugs
For the symptomatic treatment of prostatitis in men, such as pain relief during urination, you can also take antispasmodics that relax smooth muscles and thus quickly relieve pain.
Anticoagulant and anti-inflammatory dietary supplements based on bee products, pumpkin seed oil, palm fruit extracts contribute to general recovery.
Diet and lifestyle
For the treatment of prostatitis, a correct and balanced diet and a healthy lifestyle are very important. Food should not contain spicy, fried, salted or pickled foods. In the acute form, alcohol is strictly prohibited.
Foods should contain enough fiber to prevent constipation. The protein content should be reduced. It is desirable to supplement the diet with herbs, ginger, pumpkin seeds.
Non-drug treatment
Non-drug methods of therapy allow you to act directly on the prostate, increase the concentration of drugs in its tissues, help eliminate congestion.
Microwave hyperthermia is performed using a rectal probe inserted into the patient's anus. On the device, you can set the temperature required for a particular type of exposure. To increase the concentration of the drug in the prostate, it is necessary to heat 38-40°C. To achieve an antibacterial effect - 40-45 ° C.
Today, non-drug treatments focus on laser therapy. The possibilities of this technique are wide. Under the influence of a laser, the following processes occur in the prostate:
- activation of redox reactions;
- improves blood microcirculation;
- new capillaries form;
- pathogenic microflora is suppressed;
- the process of cell division is activated, which contributes to the regeneration of tissues.
During the period of research on the effects of laser therapy on patients with prostatitis, a side effect, but positive for the purposes of treatment, was found. In those who completed the course, potency increased, erectile dysfunction was eliminated, and vitality was restored. To achieve this result, it is necessary to use a beam of a certain wavelength. In general, low intensity laser radiation is used to treat chronic prostatitis.
Patients can, on their own initiative, undergo laser treatment, if it is not prescribed by the attending physician.
Surgical treatment of chronic prostatitis
Chronic prostatitis does not pose a threat to the patient's life, but can significantly reduce its quality. The most serious complication of this disease is the formation of stones in the tissues of the gland. In order to free it from the prostoliths, a transurethral resection is used.
The surgery is performed under the supervision of TRUS.
If complications such as sclerosis of the prostate occur, transurethral electrosurgery is performed. If, in combination with this pathology, sclerosis of the neck of the bladder is observed, a partial resection of the prostate is performed.
With the blockage of the seminal and excretory ducts, endoscopic operations are indicated to eliminate violations of the patency of the secret. For this purpose, an incision is made in the seminal vesicles and excretory ducts. With an abscess, complete removal of the gland is possible.
Consequences of untreated prostatitis
Even if the symptoms of prostatitis do not appear for a long time, it is necessary to be regularly examined by a urologist. Not completely cured prostatitis can be accompanied by the formation of calcifications, which then need to be removed together with the gland. Experts are sure that there are no other ways to remove or dissolve the stones.
In addition, pathogenic microorganisms can migrate to nearby organs, causing inflammation. Running prostatitis can provoke the development of adenoma and prostate cancer.
Forecast and prevention
Acute prostatitis is a disease that has a strong tendency to become chronic. Even with timely and adequate treatment, more than half of patients end up with chronic prostatitis. Recovery is far from always achieved, however, with the correct and consistent treatment and following the doctor's recommendations, it is possible to eliminate unpleasant symptoms and achieve long-term stable remission in a chronic process.
Prevention consists of eliminating risk factors. It is necessary to avoid hypothermia, to alternate sedentary work and periods of physical activity, to eat regularly and fully. For constipation, laxatives should be used. One of the preventive measures is the normalization of sexual life, since excessive sexual activity and sexual abstinence are risk factors in the development of prostatitis. If symptoms of a urological or sexually transmitted disease appear, you should consult a doctor in a timely manner.





























